In the intricate landscape of health policy, the sudden disenrollment of millions from Medicaid in 2023 remains a significant puzzle.
Utah, like several other states, witnessed a substantial reduction in Medicaid coverage after a three-year hiatus prompted by the COVID-19 pandemic.
A recent survey obtained by KFF Health News from Utah state officials provides valuable insights into this enigmatic phenomenon.
Procedural Quandaries: Decoding Disenrollments
Over 13.3 million people nationwide faced disenrollment from Medicaid in 2023, and a staggering 70 percent of these cases were attributed to procedural reasons, such as missing paperwork, according to KFF.
Utah, too, experienced a substantial reduction in Medicaid beneficiaries, leading to the question: What prompted these procedural terminations?
The Utah Survey: Shedding Light on Disenrollment Trends
A survey conducted in October, comprising over 1,000 disenrolled Medicaid beneficiaries in Utah, revealed intriguing findings.
Astonishingly, 57 percent of those who left the program in 2023 did not attempt to renew their coverage.
While the reasons behind procedural terminations remain unclear, this study provides a closer look at the human side of the issue.
Pathways Beyond Medicaid: Where Did They Go?
The silver lining in this scenario is that a significant number, 39 percent, found alternative insurance through employers, and 15 percent availed coverage through the Affordable Care Act marketplaces, as per the study.
However, the downside is that 30 percent became uninsured, facing obstacles in reapplying for Medicaid, a crucial safety net for low-income individuals and those with disabilities.
Barriers to Reapplication: A Complex Web
For the 30 percent who became uninsured, the journey back to Medicaid proved challenging.
The study identified various barriers, including 19 percent who claimed to never receive renewal documents from the Utah Medicaid enrollment agency.
Additionally, 14 percent cited procrastination, 13 percent found the process too complicated, and 7 percent lacked the necessary documents to prove eligibility.
Communication Breakdown: Struggles with the State Medicaid Agency
The study highlighted the difficulty unenrolled individuals faced in getting their questions answered by the state Medicaid agency.
While 39 percent reported resolving their issues on the same or next day, a concerning 12 percent waited more than two weeks, and 21 percent claimed their concerns were never addressed.
Clearly, there are communication gaps that need addressing.
The Renewal Process: A Daunting Task for Many
Half of those deregistered characterized the renewal process as difficult, with only a quarter finding it easy. This sheds light on the challenges faced by Medicaid beneficiaries in navigating the reapplication procedure.
The online survey, with a margin of error of plus or minus 3 percent, underscores the need for streamlined processes and improved communication channels.
Pandemic Impact: The Unfrozen Eligibility Checks
The mandatory yearly eligibility review for Medicaid beneficiaries was halted in March 2020, freezing checks due to the pandemic.
While this ensured no immediate disenrollments, the aftermath has been a reassessment of eligibility across states.
Since the spring, states, including Utah, have been reevaluating Medicaid eligibility, resulting in the ongoing “settlement” expected to continue through May.
Utah’s Perspective: Flaws and Improvements
Utah’s significant drop of about 150,000 Medicaid beneficiaries since April raises eyebrows.
Stephanie Burdick, a Medicaid enrollee and consumer advocate, pointed out serious flaws in Utah’s approach, emphasizing a communication error.
Many beneficiaries, she noted, were unaware of the need to reapply, assuming it was a one-time benefit similar to federal stimulus checks.
Jennifer Strohecker, Utah’s Medicaid director, acknowledged the feedback from the survey, stating it is instrumental in enhancing consumer engagement.
Initiatives include extending eligibility through database verification of income and residency and facilitating registrations at unconventional locations like laundromats and Department of Motor Vehicles offices.
Economic Landscape: Explaining Disenrollment Numbers
Utah’s strong economy and low unemployment rate are posited as potential explanations for the high percentage of people discharged from Medicaid.
Kevin Burt, deputy director of the Utah Department of Human Services, predicts that about 35 percent of those disenrolled will return to the program.
Conclusion: Navigating the Complex Landscape of Medicaid Disenrollments
The Utah study provides a nuanced understanding of the Medicaid disenrollment phenomenon, uncovering challenges, and shedding light on potential solutions.
Communication gaps, procedural hurdles, and the complex renewal process are all contributing factors, and addressing these issues is crucial for ensuring the seamless functioning of Medicaid programs.
Practice Yoga at Home: A Comprehensive Guide for Beginners to Advanced
Uncover the secrets of practicing yoga at home. From beginner poses to advanced routines, learn how yoga can enhance your…
Acid Reflux: Effective Strategies for Relief and Prevention
Are you experiencing acid reflux pain? You are not alone yourself. Millions of individuals worldwide suffer from this common yet…
Physical activity protects breasts from cancer before menopause
A look at ‘Physical activity protects breasts from cancer before menopause’ For women navigating the years before menopause, a new…
Understanding 5 Types of Fatigue in 2024
Fatigue, often dismissed as a fleeting concern, is more nuanced than a simple remedy of a short nap or a…
Drinking Water – A Lifesaving Elixir
Drinking water is often underestimated, but a groundbreaking study by the National Institutes of Health (NIH) reveals its profound impact…
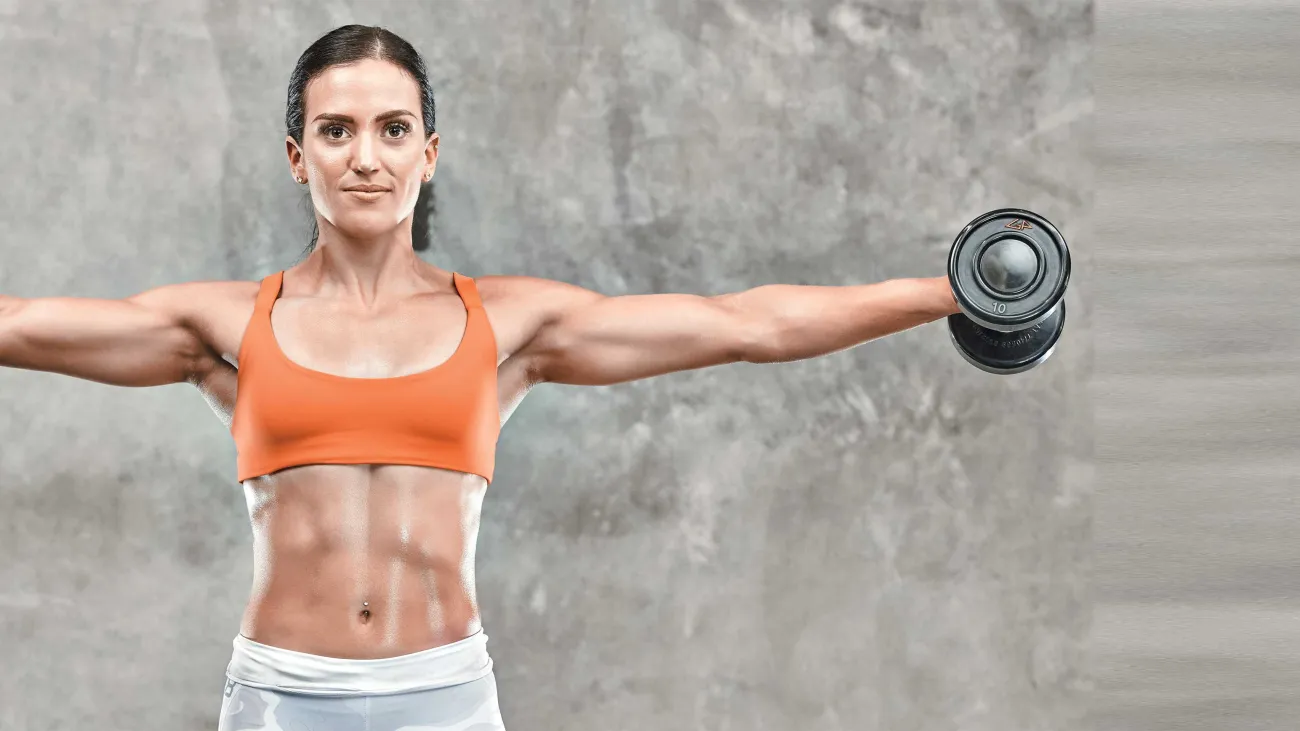
The Ultimate Showdown: Women Fitness Workouts
In the quest for a healthier and more vibrant life, the journey to fitness often stands at the forefront. For women…






Thanks for sharing. I read many of your blog posts, cool, your blog is very good.